First hand experiences
On this page
Dr Adelene Houlton
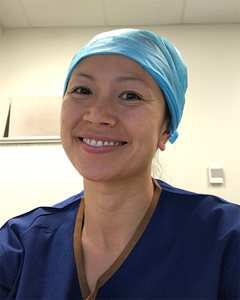 Access to flexible training enabled Dr Adelene Houlton to continue her progress towards Fellowship after six months parental leave. She returned to training in a 0.5 EFT role for 12 months and is now back in full time training.
Access to flexible training enabled Dr Adelene Houlton to continue her progress towards Fellowship after six months parental leave. She returned to training in a 0.5 EFT role for 12 months and is now back in full time training.
“I definitely went forward in this part time role, both with my knowledge and technical skills,” Dr Houlton said.
Support from the rest of the surgical team and extra attention to communication were among the things that made flexible training work, she said.
“The department was really supportive of my learning and was very accommodating,” she said.
Professor Deborah Bailey had created the stand-alone flexible role, by reallocating unit overtime. The role was carefully structured to meet RACS training requirements, including leadership opportunities and to meet the unit’s clinical need. Dr Houlton was the senior trainee on the team, supervising a full-time unaccredited registrar.
“Even though I wasn’t there all the time, I was still able to be the senior trainee, which was a really great learning experience, with input from consultants,” Dr Houlton said.
Dr Houlton and the registrar set up an extra phone call at the end of each day, to facilitate handover and debrief about complex cases.
“It was a very supportive arrangement and there was a lot of knowledge transfer between the team. The call made me more prepared for the next day’s work and was helpful to both of us,” Dr Houlton said.
“Other junior doctors never said anything about me not being there and all the teams worked well. The team seemed to like that I was part time, and had two children and a life outside work,” she said.
One of her scheduled shifts was a training afternoon with departmental teaching , which Dr Houlton organised for the year. It included consultant led teaching off the wards and lectures and audit with other departments in Queensland. There was a teaching afternoon every week which gave the other junior doctors a valuable opportunity to see a Trainee being taught.
Dr Houlton said flexible training made her more efficient at work and when doing things related to work. “I got things done smarter and quicker when I set my mind to it. The rest of the time was family time,” she said.
“If I hadn’t had access to flexible training, I would have had to take more time off, probably a full 12 or 18 months,” she said.
Dr Houlton initially approached the Chair of her Training Board, when she was pregnant with her first child.
“I asked about taking a year off, and he said great, congratulations, your options are flexible and you can do whatever you like. If you want three months off and then come back part time, we can make that work. Have a think about it and let me know in two weeks. I was blown away. I didn’t think the hospital was willing to do it. I didn’t think the Board would do it.”
At the time, Dr Houlton went back to full time training after a break, and then opted for flexible training after her second child. She has now returned to full time training after a year of working flexibly, because ‘otherwise it would have taken too long’.
Knowing there is support from ‘the top’ was critical and gave Trainees the confidence to ask about flexible training options.
“I would definitely recommend it to other people, it was good for me as a Trainee to continue at a pace I was really comfortable with. I was also able to continue breast feeding longer than would have been possible if I’d been full-time,” she said.
Professor Deborah Bailey

Professor Deborah Bailey has long been an advocate for flexible training. She created a stand-alone, flexible role in her unit before she had received any request from Trainees.
“Many surgical units in Australia are really busy and the registrars do a lot of overtime. It makes sense to have a half time role, independent of a job share partner. One registrar does part time, and the other registrars do less overtime,” Professor Bailed explains.
Trying to find two people in the same place in the same specialty is one option to do flexible training, but Professor Bailey felt there had to be another way.
“Especially when there is a role that more than one person could do – that’s the ideal opportunity to get a half time person,” she said.
“It is possible and it can be done within an existing budget envelope. It’s safe for patients and it’s great for Trainees,” she said.
The big issues with flexible training are consistency, continuity and competency progression, she says.
“We have to have consistency and continuity for patients, from admission to discharge.Trainees also need to work that journey from admission to discharge. The Trainee needs contact with the supervising consultant, in order to see the Trainee work across a range of scenarios, monitoring and mentoring them, bringing them up from one level to another. The consultant needs to get a feel for the Trainee’s progress,” Professor Bailey said.
Professor Bailey says it is ‘totally possible’ to make progress and measure progression of surgical competencies in a flexible role. As an adult learner, the Trainee has to drive the assessment and the learning.
“Loads of formative assessment is essential. Every time the trainee was at the hospital we did some formative assessment, formal teaching that worked very well. Over 12 months, the Trainee progressed from one level to the next. The Trainee was extremely satisfied and it worked well for the unit,” she said.
The job of consultants is, in part, to ensure competency progression in the trainees they are supervising.
“When you’ve identified some things the trainee is not getting experience or progress in, leadership skills for example, then you make sure everything is a leadership opportunity. It takes leadership to make handover work. One Trainee made sure that every time she operated was a formative assessment, a formal process of teaching. There is a specific task, the Trainee does it, you give formative assessment in a detailed conversation post- operatively for five minutes. You make a formal record, from which it’s then easier to compare. That’s how we assess all our Trainees and it applies to flexible training,” she said.
Professor Bailey designed the timetable so the Trainee only worked for one or two bosses at a time, and their schedules were in sync. Another key to the success of the role was shared commitment to a common goal.
“I decided to make flexible training happen. We wanted it to work. We wanted to be leaders. And we had bosses and juniors committed to making it work,” Professor Bailey said.
“You have to build a role that trainees will succeed in, not one built to fail. Supervisors may need to be a bit more focused on their teaching, may need to adjust their timetable a bit to make it work,” she said.
Professor Bailey believes that all trainees need some full-time chapters. “Some patient journeys take more time, and it takes time to learn complex surgery. The more advanced the Trainee, the harder it is to make competency acquisition – in technical and non-technical skills, medical, clinical decision making, situational awareness,” she said.
She says establishing a flexible role requires investment and effort. “It involves careful planning, getting it through hospital HR, more formative assessment, attention to handover, …you have to be interested and involved,” she said.
Mr Jonathan Karpelowsky
 The Board of Paediatric Surgery holds strong views about the importance of flexible training. Former Board Chair, Mr Jonathon Karpelowsky, says the Board believes that any centre with more than one Trainee needs to offer flexible training.
The Board of Paediatric Surgery holds strong views about the importance of flexible training. Former Board Chair, Mr Jonathon Karpelowsky, says the Board believes that any centre with more than one Trainee needs to offer flexible training.
“There’s a perception in some places that flexible training is difficult and it gets put in the too hard basket – but surgical training, certainly in paediatric surgery, is competency based and some training is better than no training,” Mr Karpelowsky said.
Access to flexible training should not be a gender issue, he said.
“Two thirds of paediatric Trainees are women – but gender shouldn’t matter,” Mr Karpelowsky says.
“You need to do it, because it’s in the RACS accreditation standards. Our Board expects that if a Trainee requests flexible training that supervisors and seniors will work out how to make that happen,” he said.
He notes there is also an economic incentive: flexible roles reduce overtime. As well, there is a range of options for structuring a flexible role.
“A job share doesn’t have to be split between two accredited Trainees. It can also be .5 accredited Trainee and .5 unaccredited registrar,” he says.
It’s also possible to adjust the clinical time to maintain exposure for Trainees, so some roles are .6 or .7. It can be cost neutral, to add to the staff count with an additional flexible role and reduce overtime or find a .5 + .5 job share.
In larger units, there may also be an option to absorb the balance between a full-time and flexible role, but that’s not possible everywhere, he said.
“In our experience, once a team has gone through the experience of flexible training, it’s positive for everyone,” he said.
Of course, there are challenges. As a supervisor, you ‘have to get your head around assessment’ and the trajectory of progress may be flatter than full time training.
“We also try to avoid having exclusively fractional or part time people in our unit, because if there’s no overlap sometimes handover doesn’t work as well and that can be a challenge.
“In bigger units, one full time and one fractional can work well to provide continuity of care,“ he said.
Dr Joanne Dale
 Dr Joanne Dale supports flexible training, but acknowledges that it’s not ‘one-size fits all’ for all departments, surgeon-supervisors and Trainees.
Dr Joanne Dale supports flexible training, but acknowledges that it’s not ‘one-size fits all’ for all departments, surgeon-supervisors and Trainees.
She observes that many surgeons without an experience of flexible training are hesitant about the concept, but argues that a well-designed training post makes it a positive experience for all.
“All flexible Trainees are juggling various commitments and are acutely concerned that they do a good job as a Trainee,” she says.
Dr Dale says flexible training is not appropriate for the whole duration of training, because you still need concentrated periods of experience and immersion into the surgical community to satisfactorily complete training.
Dr Dale completed her own training full time and is now a working part-time as a Colorectal Surgeon. Working less than five days per week suits her life at this stage. She is currently completing a Masters degree, has two young children, works clinically three to four days per week and has an academic university appointment.
An advocate for flexible training, she encourages surgical units to be creative, and consider the creation of stand-alone part time positions and not just job share arrangements.
“By having a flexible Trainee in General Surgery, you have them for 12 months. This continuity within the unit is underrated,” she says.
‘The problem with one week on, one week off is that it is totally unworkable for childcare, doesn’t work for ill health or the pursuit of elite sports,’ she said.
“We have had Trainees recovering from the effects of cancer treatment, when working a 50-60-hour week is not feasible,” she said.
Other flexible options involve splitting a full-time role between an unaccredited registrar and an accredited Trainee, two days and three days per week, or creating a stand-alone part time role.
“Our unit has a 0.4 FTE unaccredited registrar, a 0.6 FTE accredited RACS Trainee and 1.0 FTE Fellow, with three part time consultants and it works well,’ she said. The unaccredited registrar is a junior doctor who the unit is supporting to complete a research higher degree, typically a Masters (or PhD).
“Consistent supervision of the Trainee is critical – if you’ve got a full-time Fellow in the unit, you can structure it any way you like and still get consistent supervision. The Fellow needs to be on board and supportive. You need to set the post up to succeed,” she says.
Dr Dale’s experience at the Mater Hospital Brisbane proves that flexible training roles are viable in a high activity, sub-specialty General Surgery Unit. By having two part-time positions, overtime is reduced for the unit, which also pleases HR.
She is concerned that there is too much focus on why someone might want flexible training, and not enough on creating quality flexible roles.
“There are many reasons a person could be interested in flexible training and their reasons shouldn’t matter,” Dr Dale says.
“Of the Trainees I’ve known who have undertaken flexible training, sometimes it’s been for family reasons (childcare, to support a partner, care for parent/partner), to pursue elite sports, to complement a research project, or due to illness, like recovering from cancer treatment,” she said.
“Trainees have a right to flexible training and our responsibility as trainers is to support the progression of Trainees,” she says.
Setting a flexible role up for success is vital, she says.
It is important to build learning opportunities into the flexible training experience. In general, there are fewer opportunities when you work fewer hours so this needs to be considered to ensure quality training experience. Issues of handover and continuity of care are increased in a flexible arrangement, so the management of handover is critical and must be explicitly addressed during orientation. The responsibilities for on-call and weekend ward rounds needs to made clear to all parties.
Dr Dale is concerned that some Trainees believe there is stigma attached to flexible training.
“From a Training Committee perspective, flexible trainees are well recognised as organised and hard-working Trainees. They are self-motivated and do well juggling multiple commitments,” she said.
“Some people trying to get onto the training program think it looks bad on your CV to do part time work. But that fear is unjustified,” Dr Dale said.
“If working part-time enables you to complete research, look after your family, keep you well and happy, then these things will make you a better surgeon,” she says.
Dr Dale urges her colleagues ‘not to wait until your State Training Committee forces you to create a flexible training post’.
“Since introducing flexible posts, I get multiple expressions of interest in the positions.
I am proud that in 2020, the Mater Hospital Brisbane is supporting a non-training surgical registrar completing a PhD along with our flexible colorectal training registrar. In 2021, we will be supporting a SET 3 Trainee doing a PhD working one day per week and another flexible Trainee working three days per week,” she said.
“The presence of flexible training positions permits our unit to support surgical research, to reduce registrar overtime and fatigue and importantly to support trainees to complete surgical training,” Dr Dale said.
Dr Melissa Bochner, Mr Robert Whitfield and Dr Eu Ling Neo
Arguably, South Australia punches above its weight in providing flexible training. There are several, established flexible roles in the state. The Royal Adelaide Hospital’s breast unit has had a flexible role in place since 2007 which has been available for trainees most years since. Breast and Endocrine surgeons, Dr Melissa Bochner and Dr Robert Whitfield are both senior consultants in the unit with a long and strong commitment to flexible training. Dr Eu Ling Neo was the first trainee to take the unit’s stand-alone flexible training role and now works at the Royal Adelaide as a consultant hepatobiliary and pancreatic surgeon.
Dr Melissa Bochner
Breast and Endocrine surgeon, Dr Melissa Bochner said successive senior surgeons had been committed to establishing and maintaining the flexible role in their unit, over more than a decade.
“The early credit needs to go Dr Susan Neuhaus, a surgical oncologist who set up the part time role. When she joined the unit, the unit was increasingly busy. She put a business case that the workload would be well served by adding a trainee and it was good for the unit and good for patients.
“We had enough work to support a part time Trainee, so we reallocated overtime to create a stand-alone flexible role,” she said.
“If there is no part time person, we have gaps in our service. This isn’t a supernumerary role.
“And there has to be value to the hospital. You have to be able to justify the Trainee's employment in terms of the number of shifts, the number of on call sessions, number of patients, the number of clinics attended, the operating lists. Hospitals won’t pay for a non-contributor and the Board of general surgery won’t accredit a post if there’s not enough clinical experience,” she said.
“Now the role is in place, the unit doesn’t have much overtime, it is cost effective, there is limited unrostered overtime generated. Importantly, the unit has enough work to support the extra role,” she said.
The part time role is allocated to the unit actively and independently of what the other Trainee is doing. There are clear roles which are independent of each other so the trainees are not competing with each other for work.
The role is half time role, with 2.5 days allocated in a dedicated roster. The role reflects training needs – theatre experience, clinic time, on call experience and exposure to MDT, meetings and education. It’s a fixed roster.
“It’s not confusing for the trainee or the consultants and other team members, because you know who is rostered on,” Dr Bochner said.
“The reality in 2020 is that everyone is part time. At any given time, across the hospital, a patient is more likely to be looked after by someone covering for their home team.
“In the old days, we worked 36-hour shifts and that doesn’t happen now. All the current rostering is less than full time compared to the old days!”
There is also no evidence to support the contention that you need to do something more often in a shorter time frame to learn it. In part-time training, when the role is 0.5 EFT, the rotation takes 12 months not six months, she says.
Dr Bochner believes it is good for the unit to have different trainees at different levels, because ‘everything is a learning experience for someone’.
“You have to have a Trainee on every list and every clinic helps with workflow. Also, a teaching environment can be good for the unit,” she said.
Dr Bochner said there were several keys to success.
“You have to develop a timetable that meets training needs, and has enough operating time, clinical time, on call, meetings and education.
“Thought has to go into it, to make sure handover and continuity are addressed,” she said.
Handover with a flexible role is no more difficult than with anyone else, she says.
“The handover routine is part of hospital life – you have to have a unit that collaborates; communication and teamwork are really important. There are plenty of opportunities to communicate and having a part time trainee has never been a problem,” she said.
The unit uses email, text, phone and WhatsApp as well as face to face to support handover and continuity of care. There is a lot of organisation and advance planning.
The experience of their unit shows that flexible roles are desirable for a range of reasons, including family, health, avoiding burnout, research commitments, and other interests like music or sport.
“You have to put your money where your mouth is. You have to make an effort to do something to allow people to choose part-time if that would work for them at that time, for whatever reason. It shouldn’t matter why a trainee wants flexible training,” she said.
She said the role is also great for someone who is not on the training program.
“Our unit has a Fellow, an accredited Trainee and an accredited part time Trainee. If there are no takers for the part time role, you can fill it with an unaccredited registrar and when they’re in the training program, it can sometimes be retrospectively accredited if and when the Trainee gets onto the training program,” she said.
“You need to make sure the person meets all the requirements and the logbook is up to date and reflects their experience,” she said.
Rostering is critical, and needs to ensure the part time trainee is able to attend unit meetings for audit and scientific presentations.

Mr Robert Whitfield
Mr Robert Whitfield says flexible training posts must ensure the quality of the training experience.
“We’ve always worked hard to ensure that we provide a good training experience, with good volume and access to cases. We want to be sure the experience is worthwhile and that it isn’t a second rate job,” he said.
“If in any year there’s no interest from an accredited trainee, then a non-accredited trainee can get the clinical practice and use the flexible role to bring up their experience and help secure a place on the training program,” Dr Whitfield said.
Establishing and maintaining the role has not been without its challenges, including at times limited buy-in from hospital administration.
He says planning is key, including ensuring there is no competition for cases between the full time and flexible trainees, by allocating them to separate lists.
He acknowledges there can be concerns among surgeons without experience of flexible training, including about managing underperformance, managing handover and ensuring continuity.
Acknowledging the challenges involved in managing an underperforming trainee in a flexible role, on balance Mr Whitfield believes these are not materially different from dealing with underperformance in a standard role.
“I have also heard some expressions of concern about continuity of care, but that hasn’t been a problem – the whole health system runs on handovers now, so it’s not a huge barrier,” he said.
He says the reasons someone seeks flexible training are not relevant.
“I’m on the SA training committee and I don’t ask why someone wants to be part time. It shouldn’t make any difference. It’s sometimes, but not only, for work-life balance. It can be research, music, sport, it shouldn’t matter. We need to understand there are a range of different motivations, and it increases diversity which is good for our profession,” Mr Whitfield said.
“It’s a reputational thing. We don’t want to be seen as old white guy dinosaurs that can’t embrace something modern and flexible for the workplace. We want to be seen in a different way. We need to walk the walk, not just talk the talk.”
He encourages anyone thinking about establishing a flexible role to look at the volume and caseload of the unit. It has to be real and it has to provide value to the hospital.
“You have to set up the position in good faith and it has to work for everyone. Supernumerary positions are no good for anyone. If you’re not providing a real service, you don’t feel good about yourself,” he said.
The flexible role has to be a central part of the team. Just because the trainee is not there all the time, doesn’t mean they’re not an important part of the team. The job needs to be important to the overall function of the unit.
Mr Whitfield suspects that barriers to establishing flexible training roles often emerge due to competing priorities between RACS and hospital administrators. ‘You have to prove to the hospital that it is cost effective and prove to RACS that it is training appropriate,’ he said.
“Can you create a position that meets accreditation standards? You also need to be able to negotiate with hospital business managers and accountants. If you are looking at converting a full-time role to one or more flexible positions, for example, it’s important to ensure that the overall employment costs to the hospital don’t go up, or it won’t be approved.”
Dr Eu Ling Neo
 Dr Neo was the first to take up a flexible training role in the Breast and Endocrine unit at the Royal Adelaide hospital in 2007, and now works there as a senior surgeon.
Dr Neo was the first to take up a flexible training role in the Breast and Endocrine unit at the Royal Adelaide hospital in 2007, and now works there as a senior surgeon.
“I had my first daughter before I started training, and then joined the training program when she was 10 months old.
“I did two years full time and took a year off when I had my second daughter, and then returned half time.
“In that role, I had time for reading (which every registrar has to do) and attended evening tutorials. Progressing through my training was not an issue. I was doing one list – not two. You don’t deskill if you have the right attitude – you might go up six months of skills over the 12-month rotation,” she said.
“I did a stand-alone part time role. A full-time role can be allocated to two people, but they have to work well together.”
